Skinny BBL + lipo 360 : Mastering the Art of Body Contouring
16 janvier 2026Are PEEK implants good for gonial implants ?
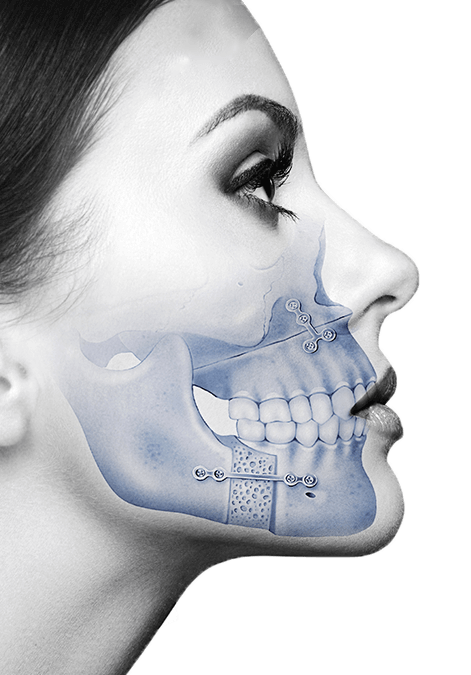
Double jaw surgery is a highly specialized surgical procedure performed by oral and maxillofacial surgeons to correct significant skeletal and dental irregularities of the jaws and face. It involves repositioning the upper jaw (maxilla), lower jaw (mandible), or both, to improve facial aesthetics, occlusal function, speech, and breathing.
Double jaw surgery is a profoundly impactful procedure that corrects fundamental skeletal and occlusal discrepancies. However, the journey to optimal facial harmony often benefits from a refinement phase. PEEK implants, with their exceptional biocompatibility, mechanical properties, and unparalleled customizability through 3D virtual surgical planning, have emerged as a leading solution for addressing subtle yet significant aesthetic deficiencies after orthognathic surgery.
By allowing surgeons to precisely augment specific craniofacial regions such as the mandibular angles, chin, and malar eminences, PEEK implants enable the creation of highly individualized and natural-looking contours. This precision translates into predictable outcomes, enhanced facial balance, and ultimately, a higher degree of patient satisfaction. While the procedure demands meticulous planning and specialized surgical expertise, the benefits of achieving refined, long-lasting aesthetic improvements make PEEK implant surgery an invaluable tool in the armamentarium of modern craniofacial and oral and maxillofacial surgeons. As technology continues to advance, the role of custom PEEK implants in perfecting post-orthognathic facial aesthetics is only set to grow.
Common Orthognathic Procedures
- Le Fort I Osteotomy: Repositions the maxilla. Used to correct an underdeveloped upper jaw, open bite, crossbite, or gummy smile.
- Bilateral Sagittal Split Osteotomy (BSSO): Repositions the mandible. Used to correct a protruding or receding lower jaw.
- Genioplasty: Repositions the chin bone. Often performed concurrently with BSSO to enhance chin projection or reduce its prominence.
Goals of Orthognathic Surgery
- Functional: Achieve a stable and functional bite, improve chewing efficiency, resolve temporomandibular joint (TMJ) disorders, and alleviate obstructive sleep apnea.
- Aesthetic: Improve facial balance and symmetry, enhance facial proportions, and create a more harmonious profile.
Despite meticulous planning and execution, the primary focus of orthognathic surgery is skeletal repositioning to correct the bite. While significant aesthetic improvements are often a direct consequence, the underlying bony structure may not always perfectly match the patient’s ultimate aesthetic aspirations or address all soft tissue contours. This is where refinement procedures become invaluable.
PEEK Implants in Craniofacial Surgery
Polyetheretherketone (PEEK) is a high-performance thermoplastic polymer that has gained significant traction in medical implantology due to its unique properties. Initially used in spinal and orthopedic surgery, its application has expanded considerably into craniofacial and maxillofacial reconstruction.
Properties of PEEK:
- Biocompatibility: PEEK is highly biocompatible, meaning it is well-tolerated by the body and elicits minimal inflammatory or foreign body reactions. This reduces the risk of adverse tissue responses and implant rejection.
- Mechanical Properties: PEEK possesses mechanical properties (e.g., modulus of elasticity, strength) that are closer to cortical bone than many other implant materials like titanium. This « bone-mimicking » characteristic helps distribute stress more evenly, potentially reducing stress shielding and bone resorption around the implant.
- Radiolucency: Unlike metallic implants, PEEK is radiolucent, meaning it does not create significant artifacts on X-rays, CT scans, or MRI. This is a crucial advantage for post-operative imaging, allowing for clear visualization of underlying bone structures and assessment of healing without obscuring details.
- Sterilizability: PEEK can be easily sterilized using standard methods (e.g., steam sterilization) without degradation.
- Customizability: Perhaps its most significant advantage in craniofacial surgery is its ability to be precisely custom-milled from 3D digital models. This allows for the creation of patient-specific implants that perfectly conform to the underlying anatomy and achieve precise aesthetic contours.
- Durability and Stability: PEEK is a robust and chemically stable material, ensuring long-term structural integrity and resistance to degradation within the body.
Advantages of PEEK in Craniofacial Applications:
- Patient-Specific Design: Enables highly precise aesthetic and functional correction.
- Reduced Stress Shielding: Mechanical properties closer to bone.
- Superior Post-operative Imaging: No artifact interference.
- Excellent Biocompatibility: Low risk of adverse reactions.
- Aesthetic Integration: Can be designed to blend seamlessly with existing bone contours.
Disadvantages of PEEK:
- Cost: Custom PEEK implants are generally more expensive than off-the-shelf implants or autologous bone grafts.
- Non-Resorbable: PEEK is a permanent implant. While this is often desired, it means it cannot be naturally integrated or remodeled by the body.
- Potential for Infection: Like any foreign body, PEEK implants carry a risk of infection, which may necessitate removal.
- Removal Complexity: While generally stable, removal, if required, can be more involved than for some other materials due to integration and screw fixation.
The rationale for refinement after double Jaw Surgery
Even after a technically successful double jaw surgery, several factors can lead to a desire or need for refinement:
- Residual Aesthetic Deficiencies:
- Incomplete Contour Correction: While jaws are moved, the overall facial shape might still lack ideal projection in certain areas (e.g., mandibular angles, chin, malar regions, paranasal areas).
- Asymmetry: Minor asymmetries can persist or become more apparent after major skeletal movements.
- Soft Tissue Response: The soft tissues (skin, muscle, fat) drape over the new skeletal framework. Sometimes, the soft tissue response doesn’t perfectly match the underlying bone, leading to areas of relative hollowing or lack of definition.
- Desire for Enhanced Masculinity/Femininity: Patients may desire more defined mandibular angles for a masculine look or a softer, more rounded malar projection for a feminine aesthetic, which orthognathic surgery alone may not fully achieve.
- Limitations of Bone-Only Movements:
- Anatomical Constraints: The extent to which bone segments can be moved is limited by surrounding nerves, blood vessels, and soft tissue attachments.
- Predictability of Bone Healing: While generally predictable, bone remodeling and healing can sometimes lead to minor deviations from the planned outcome.
- Patient Expectations: Patients often have very specific aesthetic goals that may extend beyond the primary functional objectives of orthognathic surgery.
- Secondary Deformities: In rare cases, unforeseen complications or healing patterns might create new minor contour irregularities.
- Aging: Over time, soft tissue laxity and bone resorption can alter facial contours, making previously subtle skeletal features more prominent or deficient.
In these situations, PEEK implants offer a precise and predictable solution to « fine-tune » the results, addressing specific areas of concern that were either not fully corrected by the initial surgery or were outside its primary scope.
Role of PEEK Implants in Post-Orthognathic Refinement
PEEK implants are strategically employed to address specific aesthetic and, occasionally, functional concerns in various craniofacial regions following orthognathic surgery. Their customizability allows for precise augmentation and contouring.
Common Areas for PEEK Implant Placement:
- Mandibular Angles:
- Concern: Often, after BSSO, especially in cases of mandibular advancement, the mandibular angles may appear underdeveloped, rounded, or lack sufficient flare, resulting in a less defined jawline.
- PEEK Solution: Custom PEEK implants can be designed to augment the posterior and inferior aspects of the mandibular ramus, creating a more angular, projected, and aesthetically pleasing jawline, enhancing facial masculinity or correcting asymmetry.
- Chin (Mental Region):
- Concern: While genioplasty (osseous chin advancement/reduction) is a common adjunct to orthognathic surgery, residual chin retrusion, asymmetry, or a desire for further projection/width may persist.
- PEEK Solution: Custom PEEK chin implants can precisely augment the mentum in three dimensions (projection, width, vertical height) to achieve the ideal chin contour and balance with the newly positioned jaws. They are particularly useful for subtle refinements or when further osseous genioplasty is not advisable.
- Malar/Zygomatic Region (Cheekbones):
- Concern: Midface hypoplasia, even after Le Fort I advancement, can sometimes leave the malar eminences appearing flat or lacking projection, impacting overall facial convexity and youthful appearance.
- PEEK Solution: Custom PEEK malar implants can be designed to enhance cheekbone prominence, create a more defined midface, and improve the transition between the lower eyelid and cheek, contributing to a more balanced and aesthetically pleasing facial structure.
- Paranasal Region:
- Concern: Deficiencies in the paranasal area (sides of the nose, above the maxilla) can contribute to a sunken midface appearance or deepen the nasolabial folds.
- PEEK Solution: Small, custom PEEK implants can be placed in the paranasal region to provide anterior projection, supporting the soft tissues and subtly reducing the depth of the nasolabial folds, complementing the results of Le Fort I surgery.
- Orbital Rims:
- Concern: In some complex cases or syndromic patients, orbital rim deficiencies may persist, affecting eye support or aesthetic harmony.
- PEEK Solution: Custom PEEK implants can be designed to augment the infraorbital or supraorbital rims, providing structural support and improving periorbital aesthetics.
- Correction of Minor Asymmetries:
- Concern: Even after bilateral orthognathic surgery, minor skeletal or soft tissue asymmetries can remain or become more noticeable.
- PEEK Solution: Custom PEEK implants are exceptionally valuable for precisely augmenting the deficient side to achieve greater symmetry and balance across the face.
Pre-operative Planning for PEEK Implant Placement
Meticulous pre-operative planning is the cornerstone of successful PEEK implant surgery, especially in the context of post-orthognathic refinement. It leverages advanced imaging and 3D virtual surgical planning (VSP) to ensure precision and predictability.
5.1. Patient Assessment:
- Comprehensive History: Detailed medical history, previous surgical history (specifically orthognathic surgery details), current medications, allergies, and social habits.
- Physical Examination: Thorough extraoral and intraoral examination, assessing facial symmetry, soft tissue contours, skin quality, existing scars, and palpating underlying bone structures.
- Aesthetic Goals and Concerns: Crucially, a detailed discussion with the patient to understand their specific aesthetic concerns and desired outcomes. This involves reviewing pre-orthognathic photos, post-orthognathic photos, and using imaging to highlight areas for improvement. Realistic expectations must be established.
- Functional Assessment: While primarily aesthetic, ensure no new functional issues are anticipated or existing ones exacerbated by implant placement.
5.2. Advanced Imaging:
- Cone Beam Computed Tomography (CBCT) or Medical CT Scan: This is the most critical imaging modality.
- Purpose: Provides high-resolution 3D volumetric data of the craniofacial skeleton, soft tissues, and existing hardware (plates, screws from orthognathic surgery).
- Benefits: Allows for accurate anatomical assessment, identification of vital structures (nerves, blood vessels, dental roots), and serves as the foundation for 3D virtual surgical planning.
- Protocol: Scans should be performed with appropriate resolution and field of view to capture the entire area of interest.
5.3. 3D Virtual Surgical Planning (VSP):
This is where the magic of custom PEEK implants truly begins. VSP transforms the surgical approach from a two-dimensional estimation to a precise three-dimensional design.
- Software Platforms: Specialized VSP software (e.g., Materialise Mimics, 3-matic, Dolphin Imaging, ProPlan CMF) is used.
- Process:
- Data Import and Segmentation: The CBCT/CT data is imported into the VSP software. The bony anatomy is segmented (isolated) from other tissues, creating a precise 3D model of the patient’s skull.
- Virtual Implant Design:
- The surgeon, in collaboration with a biomedical engineer or specialized company, virtually designs the PEEK implant directly onto the patient’s 3D bone model.
- This involves sculpting the implant’s shape, volume, and contours to achieve the desired aesthetic outcome, ensuring it perfectly conforms to the underlying bone.
- Considerations include:
- Thickness and Projection: To achieve the desired augmentation.
- Feathered Edges: To ensure a smooth transition with the native bone and minimize palpability.
- Fixation Points: Predetermined screw holes are designed into the implant for secure attachment to the bone.
- Avoidance of Vital Structures: The design meticulously avoids nerve pathways (e.g., mental nerve, inferior alveolar nerve), major blood vessels, and dental roots.
- Symmetry Analysis: For asymmetry correction, the implant is designed to mirror the contralateral side or achieve a new symmetrical ideal.
- Surgical Simulation: The software allows for virtual placement of the designed implant, simulating the post-operative appearance. This enables the surgeon and patient to visualize the expected outcome, make adjustments, and ensure all aesthetic and functional goals are met before surgery.
- Manufacturing: Once the design is finalized and approved, the digital file is sent to a specialized manufacturing facility. The custom PEEK implant is then precisely milled using computer-aided design/computer-aided manufacturing (CAD/CAM) technology.
- Sterilization and Delivery: The finished implant is sterilized and packaged, ready for surgical use.
5.4. Informed Consent:
- A thorough discussion covering the benefits, risks, alternatives, and expected outcomes of PEEK implant surgery is essential.
- Patients must understand the permanent nature of the implant, potential for infection, and the need for revision surgery in rare cases.
- Realistic expectations regarding the degree of aesthetic change and potential for subtle asymmetries should be reinforced.
Surgical Procedure
The surgical placement of PEEK implants after double jaw surgery requires precision, a deep understanding of craniofacial anatomy, and adherence to sterile techniques.
6.1. Anesthesia:
- General anesthesia is typically administered for patient comfort and surgical control.
6.2. Incisions:
The choice of incision depends on the location of the implant and the surgeon’s preference, aiming for minimal visibility and optimal access.
- Mandibular Angle/Body Implants:
- Intraoral Approach: Most common. Incisions are made in the buccal vestibule (inside the mouth, near the molars). This avoids external scars but requires careful dissection to prevent injury to the mental nerve or parotid duct.
- Submandibular/Retroauricular Approach: Less common for aesthetic refinement, but can be used for larger implants or complex reconstructions. Leaves a small external scar.
- Chin Implants:
- Intraoral Approach: Incision in the lower labial vestibule (inside the lower lip).
- Submental Approach: Incision under the chin. Offers direct access but leaves a small external scar.
- Malar/Zygomatic Implants:
- Intraoral Approach: Incision in the upper buccal vestibule.
- Subciliary/Transconjunctival Approach: Through the lower eyelid. Primarily used for orbital floor reconstruction but can provide access to the malar region.
- Coronal Approach: Incision within the hairline, providing wide exposure to the midface and forehead, but is a more extensive procedure.
- Paranasal Implants:
- Intraoral Approach: Incision in the upper labial vestibule.
6.3. Dissection and Pocket Creation:
- Once the incision is made, meticulous subperiosteal dissection is performed to create a precise pocket for the implant.
- The dissection must be wide enough to allow for easy insertion and positioning of the implant but tight enough to prevent implant migration.
- Care is taken to identify and protect vital structures, such as facial nerves, sensory nerves (e.g., mental nerve), and major blood vessels.
- Hemostasis (control of bleeding) is crucial throughout the dissection to ensure a clear surgical field and minimize post-operative hematoma.
6.4. Implant Placement and Fixation:
- The custom-milled PEEK implant is carefully inserted into the prepared subperiosteal pocket.
- The implant is precisely positioned according to the pre-operative plan, ensuring its contours align perfectly with the underlying bone.
- Fixation: Small titanium screws (typically 1.5-2.0 mm) are used to secure the PEEK implant to the underlying bone through the pre-designed screw holes. This prevents implant migration, ensures long-term stability, and maintains the desired aesthetic contour. The number and location of screws depend on the implant size and location.
6.5. Closure:
- After confirming implant position and stability, the surgical site is irrigated thoroughly.
- The soft tissues are meticulously closed in layers using resorbable sutures.
- A drain may be placed temporarily if significant dissection or bleeding is anticipated, though this is less common for smaller, well-hemostased pockets.
Post-operative Care
Proper post-operative care is essential for optimal healing, minimizing complications, and ensuring long-term success of the PEEK implant.
7.1. Immediate Post-operative Period (First few days):
- Pain Management: Prescribed analgesics to manage discomfort.
- Swelling Control: Cold compresses, head elevation, and sometimes corticosteroids can help reduce swelling. Swelling is expected and will gradually subside over several weeks.
- Antibiotics: Prophylactic antibiotics are typically prescribed to reduce the risk of infection, especially with intraoral incisions.
- Oral Hygiene: For intraoral incisions, strict oral hygiene with antiseptic mouthwashes (e.g., chlorhexidine) is crucial.
- Diet: A soft diet may be recommended initially to avoid trauma to the surgical site and facilitate healing.
- Activity Restrictions: Avoid strenuous activities, heavy lifting, and any contact sports that could impact the face.
7.2. Follow-up and Monitoring:
- Regular follow-up appointments are scheduled to monitor healing, assess for complications, and remove sutures if non-resorbable ones were used.
- The surgeon will assess facial symmetry, implant position, and the patient’s overall satisfaction.
7.3. Long-term Care:
- Patients are advised to protect their face from trauma.
- While PEEK implants are highly stable, any unusual pain, swelling, or signs of infection should be reported immediately.
- Routine dental check-ups and imaging (if needed) will monitor the implant’s long-term stability.
Potential Complications
While PEEK implant surgery is generally safe and effective, as with any surgical procedure, potential complications can arise.
8.1. General Surgical Risks:
- Infection: Although rare with prophylactic antibiotics and sterile technique, infection can occur. It may manifest as pain, swelling, redness, warmth, or pus. Severe infections may require implant removal.
- Bleeding/Hematoma: Post-operative bleeding or accumulation of blood (hematoma) can cause swelling, bruising, and discomfort. In some cases, drainage may be necessary.
- Nerve Injury:
- Sensory Nerves: Temporary or, rarely, permanent numbness or altered sensation (paresthesia/dysesthesia) can occur if sensory nerves (e.g., mental nerve, infraorbital nerve) are stretched or damaged during dissection.
- Motor Nerves: Extremely rare, but injury to branches of the facial nerve could lead to temporary or permanent facial weakness or asymmetry. Meticulous surgical technique minimizes this risk.
- Anesthesia Risks: Risks associated with general anesthesia, though modern anesthesia is very safe.
8.2. Implant-Specific Risks:
- Malposition or Asymmetry: Despite meticulous planning, subtle shifts during placement or post-operative swelling can lead to minor malposition or asymmetry. This may require revision surgery.
- Extrusion/Exposure: Very rare with PEEK implants due to their excellent biocompatibility and subperiosteal placement, but can occur if the overlying soft tissue is too thin, under excessive tension, or if infection develops.
- Palpability/Visibility: In very lean individuals or with thin soft tissue coverage, the edges of the implant might be palpable or, rarely, visible. Careful design with feathered edges helps mitigate this.
- Bone Resorption (Pressure Necrosis): While PEEK’s mechanical properties are bone-like, sustained pressure from an implant on underlying bone can theoretically lead to some degree of bone resorption. This is minimized by proper implant design (smooth contours, even pressure distribution) and fixation.
- Foreign Body Reaction: Although PEEK is highly biocompatible, any foreign material can theoretically elicit a chronic inflammatory response, though this is exceedingly rare with PEEK.
- Need for Revision Surgery: In some cases, due to complications, patient dissatisfaction with the aesthetic outcome, or a desire for further refinement, revision surgery may be necessary to adjust, remove, or replace the implant.
Advantages and Disadvantages of PEEK Implants for This Application
9.1. Advantages:
- Unparalleled Customization: The ability to design patient-specific implants based on 3D imaging allows for highly precise aesthetic and anatomical correction, perfectly matching the patient’s unique contours and goals. This is a significant advantage over off-the-shelf implants.
- Excellent Biocompatibility: PEEK is well-tolerated by the body, minimizing the risk of adverse tissue reactions, inflammation, and rejection.
- Mechanical Properties Similar to Bone: Its modulus of elasticity is closer to cortical bone than titanium, potentially reducing stress shielding and preserving underlying bone integrity over the long term.
- Radiolucency: PEEK does not interfere with post-operative imaging (X-rays, CT, MRI), allowing for clear visualization of the underlying bone and surrounding soft tissues, which is crucial for monitoring healing and assessing any future concerns.
- Long-term Stability: Once fixed, PEEK implants are highly stable and durable, providing a permanent solution for contour enhancement.
- Aesthetic Integration: When properly designed and placed, PEEK implants blend seamlessly with the existing bone, creating a natural-looking and feeling result.
9.2. Disadvantages:
- Cost: The custom design and manufacturing process for PEEK implants are significantly more expensive than using off-the-shelf implants or autologous bone grafts.
- Non-Resorbable: PEEK is a permanent material. While this is often desired for structural support and long-term contour, it means the implant cannot be naturally remodeled or integrated by the body’s biological processes.
- Potential for Infection: As with any foreign body, there is a risk of infection, which may necessitate implant removal.
- Requires Specialized Expertise: Both the planning (3D VSP) and surgical execution require a surgeon with specialized training and experience in craniofacial surgery and custom implant placement.
- Removal Can Be Complex: While rare, if an implant needs to be removed, it can be a more involved procedure than for some other materials due to its secure fixation and integration with soft tissues.
Comparison with Other Materials/Techniques
When considering facial augmentation after orthognathic surgery, PEEK implants are one of several options. Understanding the alternatives helps appreciate PEEK’s unique position.
10.1. Autologous Bone Grafts:
- Description: Bone harvested from the patient’s own body (e.g., hip, rib, calvarium) and shaped to fit the defect.
- Advantages:
- Biologically Ideal: Living tissue, no foreign body reaction.
- Potential for Integration: Can integrate with the host bone.
- No Risk of Infection (Foreign Body): Less risk of infection compared to alloplastic implants.
- Disadvantages:
- Donor Site Morbidity: Pain, scarring, and potential complications at the harvest site.
- Unpredictable Resorption: Bone grafts can resorb unpredictably over time, leading to loss of volume and contour.
- Limited Volume: Amount of available bone may be limited.
- Shaping Limitations: Difficult to achieve highly precise, complex contours compared to custom-milled implants.
- Longer Operative Time: Requires a second surgical site.
10.2. Other Alloplastic Implants (Silicone, ePTFE, PMMA):
- Silicone (Solid Silicone Implants):
- Advantages: Readily available, relatively inexpensive, easy to carve intraoperatively.
- Disadvantages: Less biocompatible than PEEK, higher risk of capsule formation, potential for migration if not fixed, can feel unnatural, significant artifact on imaging.
- ePTFE (Expanded Polytetrafluoroethylene, e.g., Gore-Tex):
- Advantages: Biocompatible, soft, can be trimmed.
- Disadvantages: Less structural rigidity, prone to infection if exposed, can be difficult to remove if ingrowth occurs.
- PMMA (Polymethyl Methacrylate):
- Advantages: Can be molded intraoperatively, cost-effective.
- Disadvantages: Exothermic reaction during polymerization (risk of thermal injury), less precise than custom PEEK, can be brittle, significant artifact on imaging.
10.3. Autologous Fat Grafting:
- Description: Fat harvested from another part of the patient’s body (e.g., abdomen, thighs) and injected into the target area.
- Advantages:
- Autologous: No foreign body reaction.
- Soft Tissue Augmentation: Ideal for filling soft tissue deficiencies and improving skin quality.
- Minimally Invasive: Less invasive than bone grafting or implant placement.
- Disadvantages:
- Unpredictable Retention: A significant portion of the grafted fat may resorb, requiring multiple sessions to achieve the desired volume.
- Limited Structural Support: Does not provide skeletal augmentation or definition.
- Not for Bony Contouring: Cannot create sharp angles or precise bony contours.
Why PEEK often stands out for post-orthognathic refinement: PEEK’s ability to be custom-designed with extreme precision, its excellent biocompatibility, and its mechanical properties that mimic bone make it an ideal choice for addressing specific bony contour deficiencies after orthognathic surgery where precise, stable, and long-lasting augmentation is required without the morbidity of bone grafting or the limitations of other alloplastic materials